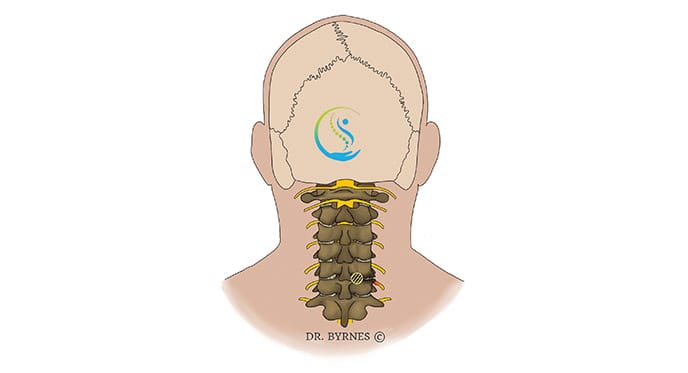
Minimally invasive cervical foraminotomy is a surgical procedure performed to alleviate nerve root compression in the cervical spine.
This minimally invasive approach involves minimal disruption to the surrounding tissues and offers several advantages over traditional open surgery.
This article will discuss the indications, techniques, benefits, and potential risks of minimally invasive cervical foraminotomy.
Minimally invasive cervical foraminotomy is primarily indicated for patients suffering from cervical foraminal stenosis, a narrowing of the foramina (openings) through which the spinal nerves exit the spinal canal.
Common causes of cervical foraminal stenosis include degenerative disc disease, spinal arthritis, bone spurs, and herniated discs.
Symptoms that may warrant this procedure include radiculopathy (nerve root compression) and muscle weakness or numbness in the arms or hands.
Minimally invasive cervical foraminotomy is performed under general anaesthesia with the patient positioned prone on the operating table. The procedure typically involves the following steps:
Minimally invasive cervical foraminotomy offers several advantages over traditional open surgery, including:
As with any surgical procedure, minimally invasive cervical foraminotomy carries potential risks, including:
Minimally invasive cervical foraminotomy is an effective surgical treatment for cervical foraminal stenosis, providing significant relief from neurological symptoms and improving the patient's quality of life.
The minimally invasive approach offers several advantages over traditional open surgery, including reduced tissue damage, faster recovery, and improved cosmetic outcomes.
However, potential risks and complications should be carefully considered and discussed with the patient and surgeon before proceeding with the surgery.
Proper patient selection, meticulous surgical technique, and comprehensive postoperative care can significantly improve outcomes and overall patient satisfaction.
