



Lumbar Disc ProlapseIntroduction: Lumbar disc prolapse, commonly known as a slipped or herniated disc, occurs when the soft inner part of a spinal disc protrudes through a tear in its outer layer.
read more
Cervical disc prolapse, or herniated disc in the neck, occurs when the inner part of an intervertebral disc pushes through a tear in the outer layer, compressing nearby nerves or the spinal cord.
read more
Lumbar epidural steroid injections (LESIs) are a common, minimally invasive treatment for back pain and sciatica, caused by conditions like herniated discs, spinal stenosis, and degenerative disc disease.
read more
Lumbar facet joint injections are straightforward injection procedures used to diagnose and treat pain thought to relate to the facet joints in the lower back, often caused by arthritis or injury.
read more
Carpal tunnel syndrome (CTS) is a common nerve compression disorder causing pain, numbness, and weakness in the hand and wrist. Non-surgical treatments are often effective in managing CTS symptoms.
read more
Mechanical low back pain (MLBP), which accounts for the majority of back pain cases, refers to discomfort resulting from a problem with the muscles, ligaments, joints, or discs of the spine.
read more
Pain-relieving medicine: Simple ‘Over the Counter’ pain relieving medication can be used without need for prescription.
read more
For patients with occipital neuralgia who have moderate to severe pain symptoms, a local Occipital Nerve Block often provides pain relief, which is .... typically prompt, supports the diagnosis and may last several weeks or even months. The procedure is generally safe and can be repeated when pain recurs.
read more
Short courses of Nonsteroidal anti-inflammatory medicines and simple muscle relaxants, may benefit patients and facilitate their participation in physical therapy.
read more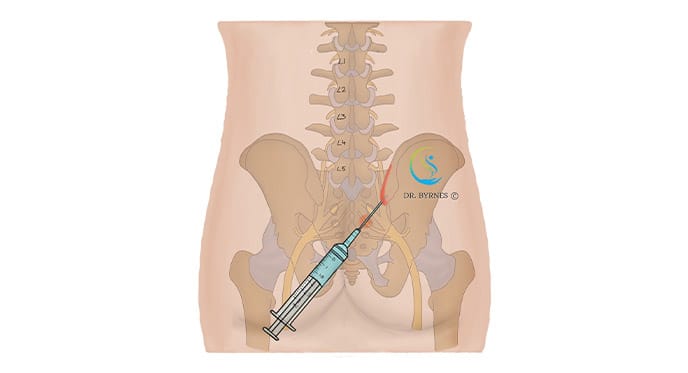
CT-guided sacroiliac joint injections are a minimally invasive procedure used to diagnose and treat pain originating from the sacroiliac joint, typically caused by inflammation or injury.
read more